The availability of ECMO may have saved lives during the height of the pandemic. In the future, it may buy patients much-needed time and give them a bridge to further treatment.
It was with this in mind that Dr. Ridwan Shabsigh, chair of the Department of Surgery, first approached Dr. Rocco Lafaro, a cardiothoracic surgeon at SBH, about developing an ECMO program for seriously ill patients suffering from respiratory or heart failure. He wanted to know what Dr. Lafaro, who has years of experience working with ECMO at other institutions, thought of the idea.
“He saw it as a way to elevate the surgery and critical care departments of the hospital and, most importantly, save lives,” says Dr. Lafaro, who agreed with Dr. Shabsigh and worked with him, the critical care team and clinical administrators in the months ahead to put the idea into motion.
In a hospital that lives under the constant financial strain of a patient population with an overwhelming percentage on Medicaid, where reimbursements are low, the administration first had to take a hard look at the numbers to determine that, at the very least, having an ECMO program would be a “financial wash,” says Dr. Lafaro. Meanwhile, while ECMO has been the standard of care for many major teaching institutions in New York City and around the country, few community hospitals offer it because the learning curve can be exceedingly steep for physicians, nurses and support staff.
“Everyone at the hospital supported the idea of bringing the program here,” says Dr. Christopher Grantham, director of critical care medicine, once the financial information suggested that a sufficient number of patients could be supported by ECMO. “We have people who end up with respiratory failure and, in the past, when we’ve wanted to transfer these patients out they were often very unstable, which is risky – even if that particular hospital is accepting transfers [which during the height of COVID-19 was not the case]. It can be lifesaving for a select group of people with the right criteria. Without it, they can end up with hypoxia to the brain and multi-organ failure. With ECMO, if you oxygenate them, could they survive? Maybe.”
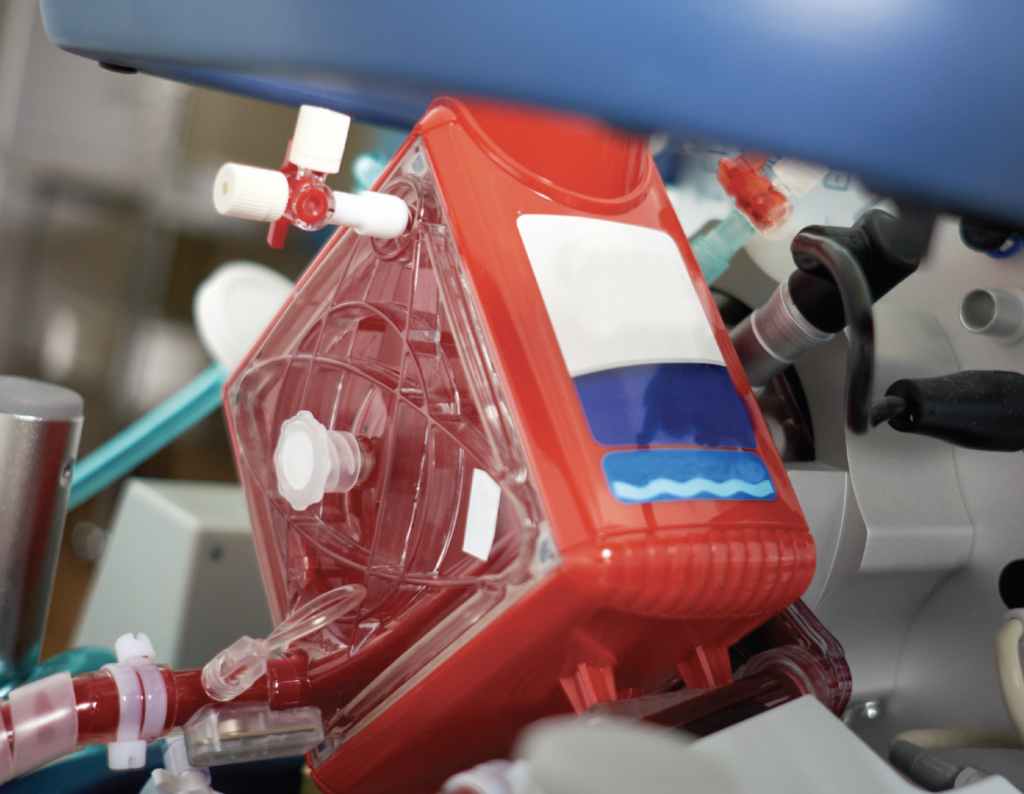
ECMO, which stands for extracorporeal membrane oxygenation, is a complex procedure where a patient is connected to a machine that functions as the patient’s external heart and lungs. The machine pumps and oxygenates the patient’s blood outside the body, taking the volume and pressure off the heart and lungs and allowing them to rest. When attached to an ECMO machine, a patient’s blood flows through tubing to an artificial lung in the machine that adds oxygen and removes carbon dioxide. The machine warms the blood to body temperature before pumping it back into the body.
The patient population most likely to use ECMO at SBH would be those ventilated who suffer from respiratory distress due to COVID-19, asthma, COPD, flu, sepsis, pneumonia and other illnesses. It could also be used for patients awaiting lung transplants or needing to be stabilized prior to being transferred to another facility.
Although not initially recommended for COVID-19 patients, later studies indicated its effectiveness, according to a recent article published in The Lancet. Data from ELSO, the Extracorporeal Life Support Organization, which keeps a registry of patient outcomes on ECMO machines, shows that the global mortality rate for COVID-19 patients treated on ECMO in recent months stands at about 48 percent. It’s considered a “Hail Mary” for those patients who have run out of other options.
The medical community views the concept behind ECMO as a simple one: allowing gas exchange to support patients with a lung injury by giving their organs a break. However, the program itself requires highly trained staff and specialized equipment. Scheduled to start at SBH in early 2022, ECMO requires a team comprised of surgeons and critical care physicians, nurses, and respiratory therapists.
Nursing will play a hugely critical role in its rollout, as the treatment requires one- to- one nursing care and close attention to the machines and factors that can range from bleeding to kidney failure. A perfusionist is dedicated to running the machine. Patients may be tethered to an ECMO machine for weeks at a time.
“It’s a saving device once you’ve exhausted all others,” says Dr. Lafaro. “It’s an intensive program and we’ll have to work hard at it. But we have good people here and I’m confident that with the support group we are putting together, we can make it work.”




